Post-Treatment Lyme disease Syndrome (PTLDS), also known as Post-Lyme Syndrome, is a condition that can occur after receiving treatment for Lyme disease.
PTLDS is a set of chronic symptoms that can persist in some individuals for months or even years after a course of appropriate antibiotic treatment. It is an infection caused by the bacteria Borrelia burgdorferi. It occurs when a person has been treated for Lyme disease, but still experiences symptoms of the infection even after the treatment is completed. People with PTLDS experience persistent and long-lasting symptoms, including fatigue, joint pain, cognitive difficulties, and sleep disturbances.
There is an alarming number of patients experiencing persistent symptoms that are disabling. The exact cause of this syndrome is unknown but is thought to have something to do with long-term changes in the nervous system caused by the Lyme bacteria or due to lingering inflammation even after treatment has been completed.
Post-Lyme Disease Syndrome (PLDS)
There is an alternate term for Post-Treatment Lyme disease Syndrome (PTLDS): Post-Treatment Lyme disease Syndrome (PLDS). In one recent scientific study, the two terms were found to be largely interchangeable, thus creating challenges and confusion in diagnosing and treating the wide variety of long-term symptoms associated with PTLDS.
Chronic Lyme Disease Syndrome
Now that we’ve gained insight into what PTLDS is, let us take a moment to delve deeper into Lyme disease Syndrome. To understand this condition, it’s important to analyze what Lyme disease Syndrome actually is. Investigating further, we can see it’s an infection with multi-systemic symptoms that come from the bacterium Borrelia burgdorferi transmitted by a tick bite or sometimes other insect bites.
The principal sign is known as erythema migrans, a bull’s-eye rash that forms at the site of the tick bite in some people. Upon studying the results more intently, various complications can develop into infectious illnesses such as malaise, arthritis, and meningitis. Thus a clear assumption of Lyme disease Syndrome merits careful examination to help determine potential treatments.
Lyme disease Syndrome is an infection caused by the bacteria Borrelia burgdorferi, which can be spread through a tick bite. It is one of the most common and widespread infectious diseases in the United States and has 20,000–30,000 confirmed cases per year since 2016 and affects people of all ages.
Symptoms can include fever and rash, joint pain, neurological deficits, and facial palsy. Disease control is essential to prevent the further spread of the disease; seeking an early diagnosis and providing prompt treatment is important for full recovery from this disease.
In the first studies on Lyme disease, the term PLDS was used for patients with Lyme disease who also had other symptoms like fatigue, joint pain, and muscle pain. A study classified these patients into four categories:
- Patients with symptoms of unknown cause who did not test positive for Lyme disease
- Patients who had a well-defined illness that was misdiagnosed as Lyme disease
- Patients with symptoms of unknown cause who tested positive for Lyme disease
- Patients with Post-Lyme Disease Syndrome
As knowledge about Lyme disease Syndrome expands, health organizations are continuing to research new ways to monitor disease progression and provide disease control strategies that target prevention and education.

Transmission
Lyme disease is an infectious disease spread primarily by the bites of an infected black-legged tick with the bacteria Borrelia burgdorferi. Deer ticks, especially in endemic areas, are the main disease vector and usually feed on large mammals such as deer or mice.
While it’s very unlikely to contract Lyme disease from casual contact with humans, insects, and animals, it can still be possible if someone unknowingly comes into contact with an infected tick or animal.
This disease can be prevented with disease control measures, which include checking for ticks after spending time outdoors, wearing protective clothing while outdoors, using insect repellent, and regularly consulting with a physician or a disease-control specialist. In addition to these measures, it is important to test for Lyme disease if you have been bitten by a tick and you notice symptoms such as fever, rash, facial paralysis, general malaise, or joint pain.

Persistent Symptoms
Post-Treatment Lyme disease Syndrome (PTLDS) can be difficult to diagnose due to its vague and fluctuating states of symptoms. Common manifestations include widespread musculoskeletal pain, joint pain, fatigue, cognitive dysfunction such as difficulty concentrating, post-exertional malaise with prolonged recovery, sleep disturbances, and continued flu-like symptoms.
These chronic symptoms can occur in waves but may last months or years despite initial treatment. With no set treatment plan available, it is important to be aware of the signs associated with PTLDS and discuss them with your doctor so you can receive the care that is right for you.
It is important for PTLDS sufferers to closely monitor their symptoms, be aware of available resources, and increase communication with their healthcare team in order to regain and maintain control of their condition. With adequate self-care and treatment, those living with post-treatment Lyme disease syndrome can find relief and improve outcomes over time.
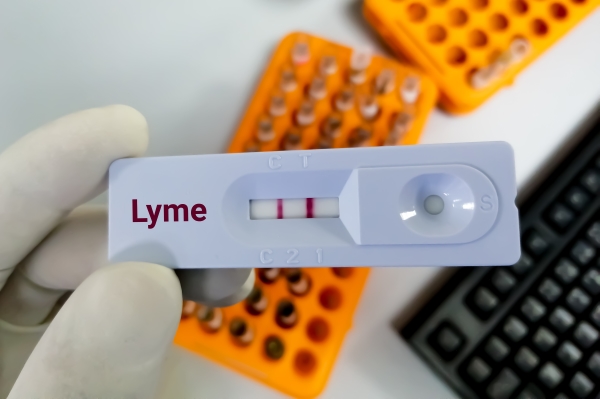
Diagnosis
Diagnosing Post-Treatment Lyme disease Syndrome (PTLDS) can be a challenge due to the complexity of its symptoms. Each patient may present with a unique set of signs and symptoms, making it difficult to easily distinguish PTLDS from other infectious diseases.
Some experts think that Borrelia burgdorferi might cause an “auto-immune” reaction. Auto-immune reactions happen when the body’s immune system attacks itself instead of the infection. Auto-immune reactions can occur after other infections, including Guillain-Barré syndrome, chlamydia (reactive arthritis), and strep throat (rheumatic heart disease).
Other experts believe that PTLDS is caused by a persistent but difficult-to-detect infection. While other experts on the other hand conclude the symptoms of PTLDS are due to other causes unrelated to the patient’s Borrelia burgdorferi infection.

Treatment Options
While there is no known cure for Post-Treatment Lyme disease Syndrome (PTLDS), short-term antibiotic treatment has been shown to alleviate symptoms of early Lyme disease. However, research has found that long-term outcomes are essentially the same for patients who have received prolonged antibiotic therapy compared to those who only get placebos.
Because of this, PTLDS can be a difficult condition to manage but current treatment options often involve antibiotic therapy, usually either an oral antibiotic or antibiotic injections which are used when there is an ongoing risk of the disease developing.
In some cases, medications like inflammatory drugs or steroids may also be used to treat certain conditions that Lyme disease has caused. Likewise, alternative methods, natural supplements, and diet changes have been found to have benefits in reducing the symptoms of PTLDS.
However, it’s important before making any medical decisions to speak with your doctor and together determine a course of treatment.
Impact on Everyday Life
Post-Treatment Lyme Disease Syndrome (PTLDS) can have significant effects on one’s everyday life. Chronic fatigue, joint pains, difficulty concentrating, headaches, and other cognitive and physical symptoms may lead to dramatic reductions in one’s quality of life. This leads to poor work function, lack of self-care, challenges in parenting, and/or an inability to pursue leisure activities.
Many individuals with PTLDS are unable to maintain gainful employment due to their symptoms. Socialization can also be difficult; in some cases, the severe fatigue experienced as part of PTLDS can make mundane tasks such as grocery shopping a challenge or exacerbate symptoms like headache or cognitive impairment.
Further Research
Post-treatment Lyme disease syndrome (PTLDS) continues to be a perplexing illness for the medical community, as research is still ongoing regarding the cause and potential treatments. PTLDS appears as a result of an overreaction of the immune system due to previous exposure to the Lyme bacteria.
The continued symptoms experienced by those with PTLDS suggest that it is an immunological disorder rather than an active infection, though further study is necessary to determine what causes these lasting effects and how they can be addressed effectively.
Despite successful treatment of past infections, PTLDS may last for months or even years afterward due to residual inflammation caused by certain proteins released by the bacteria. This can interfere with brain connectivity and disrupt cellular communication throughout the body.
Conclusion
Overall, Post-Treatment Lyme disease Syndrome can be a devastating condition for those who suffer from it. Even though there is no clear cause of PTLDS and treatments are often only moderately effective, there are a number of ways that sufferers can manage their condition.
They should consider exploring different approaches such as lifestyle modifications, medications, and alternative therapies to find the best fit for their situation.
As a consideration, the WAVE 1 bioenergetic wearable offers an alternative solution to lessening symptoms and strengthening cellular repair. Its Lyme Support Program delivered on WAVE 1 supports the energetic level of the body for immune support, addressing detox, stress and anxiety, Lyme, Co-infections, fungals (including mold), parasites, bacteria and viruses.
Support groups also provide valuable emotional support, helping them feel understood and validated in their struggles.
Taking proactive measures can give PTLDS patients the freedom to focus on regaining control, rather than passively responding to mundane medical necessities. Some helpful interventions include diet modifications or lifestyle changes that ultimately support tending to one’s own health needs.
With accurate knowledge and the right tools, those with PTLDS have the ability to take control of their lives once more and to work towards lessening or even eliminating its effects.



